IN SPITE of the 2013 Neuberger Report calling for an end of the Liverpool Care Pathway (LCP) current end-of-life ‘care’ (EOLC) pathways are continuing the LCP methodology and medications.
EOLC pathways are standard ‘care’ for those perceived as dying throughout the NHS and its nursing homes. It is claimed that these pathways do not cause death, and there have been no statistics published of patients dying on EOLC pathways because they are not mentioned on death certificates.
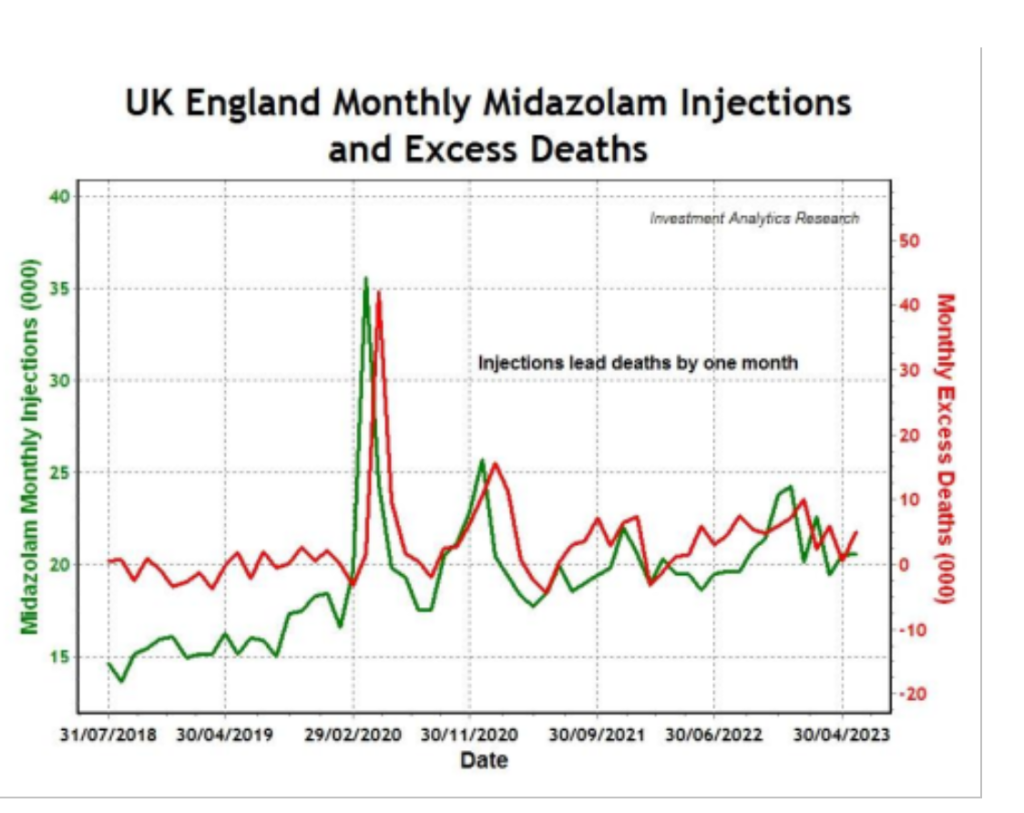
Recent research has shown that during the covid pandemic in the United Kingdom there were two major peaks of mortality, one in April 2020 and the second in January 2021.
The UK spike in deaths in April 2020, although attributed to the SARS-CoV-2 virus, was in fact because of the widespread use of midazolam injections. This conclusion is based on the very strong statistical correlation (coefficient over 90 per cent) between midazolam prescriptions and excess deaths in all regions of England.
Covid was largely absent at that time. The April 2020 peak of deaths occurred the month after release of the NG159 critical care triaging algorithm which determined that those over 65 years of age who had a clinical frailty scale of five or more (‘mildly frail: impaired shopping and walking outside alone, meal preparation and housework’) should not be admitted to intensive care and if they deteriorated should be put on end-of-life care.
The researcher concluded that the widespread and persistent use of midazolam in UK suggests a possible policy of systematic euthanasia.
Like the LCP, EOLC pathways use a combination of opiate (morphine) and benzodiazepine sedative (midazolam) delivered by syringe driver, with incremental dose increased by nurses in accordance with anticipated prescribing.
The British National Formulary (BNF) has always carried a standard warning that the combination of opiates and benzodiazepines can cause fatal respiratory depression.
Midazolam is a very powerful benzodiazepine that was only used for intractable epileptic fits or induction of anaesthesia.
More recently an indication for ‘palliative care of the imminently dying’ has been added. It is said to reduce the anxiety and agitation that may be associated with dying. Midazolam and an opiate are obligatory components of the EOLC pathway even if agitation and pain are not present.
This effectively gives a dangerous combination of drugs that might depress respiration and also is likely to cause mental confusion in the elderly. Confusion caused by these medications is likely to be managed by increasing them and thus increasing the danger of a fatal respiratory suppression.
EOLC pathways are said to be dignified and give a ‘good’ death. The appearance of ‘dignity’ or ‘comfort’ in end-of-life pathways is in major part provided by tranquillisation with midazolam. This renders the patient unable to participate in discussions, declare their needs of fluids and nutrition and, as the dose increases, gives confusion.
True dignity would be to treat without any pre-set pathway, to respect patient and relative wishes and to give best available medical care on a day-to-day basis with access to the pastor of the patient’s or family choice.
Two remaining major flaws from the LCP are firstly that it is impossible to diagnose impending death, let alone the ‘imminent’ death that the BNF requires. Research has shown that treating patients on the basis of an assumed poor prognosis leads to self-fulfilling bad outcomes.
Secondly, the Best Interest formula of the Mental Capacity Act 2005 has been shown to be ‘legal fiction’. Best interest meetings do not routinely allow the family wishes to be central despite the James vs Aintree Supreme Court 2012 legal precedent with Lady Hale concluding that this should be central.
End-of-life care pathways are a form of involuntary euthanasia. They are now effectively a forced end-of-life-diagnosing, dehydrating and life-ending machine which resists all appeals against its decisions. It is the antithesis of Christian care and must be immediately discontinued. Families must be allowed a central role in decision-making in the sick elderly.
A repeat independent review is urgently needed. The Patient Care Bill of Rights 2013 should be accepted by the NHS. In a cash-strapped NHS what will certainly happen if assisted suicide and/ or direct euthanasia is introduced is that EOLC and their practices will merge under the same staff and methodologies.
This will cause a further worsening of care of the sick elderly and quickly change ‘assisted dying’ into involuntary euthanasia on a possibly unprecedented scale.











